Cancer of the ascending colon
Patient N., 74 years old.
Height - 180 cm.
Weight - 91 kg.
Diagnosis: Cancer of the ascending colon St IIIB pT3N1 (1/19) M0 G2.
Medical history.
Routine examination for benign prostatic hyperplasia (BPH) revealed anemia.
Additional examination:
tumor markers from 16.03.16 - PSA-total - 4.22, CA19-9 - 32, CEA - 2.53, AFP - 1.35, SCC - 0.6;
CT scan of the chest from 04/03/16 - without focal pathology;
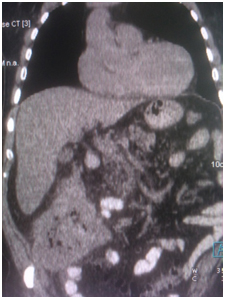
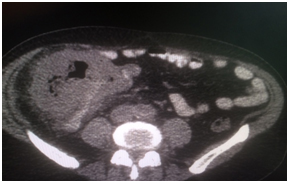
CT scan of the abdominal cavity from 03/21/16 - in the cecum, a volumetric mass up to 98 × 118 × 108 mm, paracolytic tissue is infiltrated, there are multiple lymph nodes in the surrounding tissue;
colonoscopy from 25.03.16 - a tumor of the cecum. GDz: chronic colitis.
laboratory hemoglobin - 76 g / l.
Consulted by an oncologist, surgeon of JSC "Medicine" (clinic of Academician Roitberg).
On objective examination, the condition is satisfactory. The skin is pale, clean, of moderate moisture, elastic. Peripheral lymph nodes are not palpable. No edema.
Head-neck - the thyroid gland is not enlarged.
Respiratory organs - breathing free through the nose. Respiratory rate - 17 / min. The rib cage is cylindrical in shape, evenly participates in the act of breathing. Painless on palpation. With auscultation, breathing is carried out in all departments, vesicular, no wheezing.
Circulatory organs - there is no pathological pulsation in the region of the heart, vessels of the neck and epigastrium. On auscultation, the heart sounds are muffled, rhythmic, no noise.
Digestive organs - good appetite. The abdomen of the correct shape, not swollen, participates in the act of breathing evenly. On palpation, soft. In the right half of the abdomen in the projection of the blind and ascending colon, a dense, mobile tumor up to 12 cm in diameter, moderately painful, is palpated. The liver at the edge of the costal arch. The edge of the liver on palpation is sharp, elastic, painless.
Clinical and radiological - cecum cancer.
Secondary anemia of severe severity.
Recommended:
repeat colonoscopy;
PET-CT;
irrigoscopy;
correction of hematological complications - transfusion of blood components.
Planned:
holding a consultation of the cancer center specialists;
hospitalization;
blood transfusion.
Data of laboratory and instrumental research.
Clinical blood test - hemoglobin 71 g / l.
Biochemical blood tests, clinical urinalysis - without deviations from the norm.
ECG - sinus rhythm, normosystole. The normal position of the electrical axis of the heart. Clockwise rotation of the heart (SIQIII). Nonspecific changes in the repolarization of the left ventricular myocardium.
Blood group A (II) second Rh factor Rh (+) positive.
Doppler ultrasonography of the vessels of the lower extremities - pathology of the deep veins of the lower extremities was not revealed. Insufficiency of the stem and osteal valves of both GSV. Varicose transformation of tributaries and main trunks of the GSV on both sides. Dilation of perforating veins on both sides with signs of retrograde blood flow.
Endoscopy - in the area in / 3 of the ascending colon, a volumetric tumor formation is determined, extending to the area of the hepatic flexure of the intestine, measuring 2.5-3.0 × 1.0 × 0.5-0.7 cm A biopsy (3 pieces) was performed, in which there was marked fragmentation and moderate bleeding. A stenosing tumor in the area of the border of n / 3 of the ascending colon and cecum, also when taking a biopsy (3 pieces) with severe fragmentation and moderate bleeding.
Conclusion. Tumor process of the ascending colon and cecum.
Histological examination - ulcerated malignant neoplasm of the ascending colon with the transition to the cecum with areas of complete invasion of the walls, vascular invasion, metastases in 1 lymph node from 19 mesentery of the colon, small lymph nodes and lymphoid follicles of the submucosa.
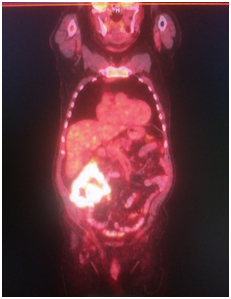
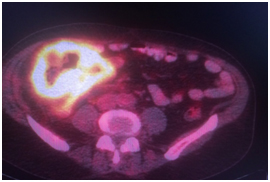
PET / CT scan was performed at 18 F -FDG.
Revealed a hypermetabolic tumor process in the cecum and ascending colon (SUVmax 21.9), the surrounding paracolytic tissue is unevenly infiltrated, with a small amount of fluid content. The intestinal lumen is unevenly narrowed. In the surrounding paracolytic tissue, the mesentery of the small intestine, there are lymph nodes up to 6-8 mm in size in KO, with a moderate accumulation of RP, SUVmax 4.3.
Conclusion of the consultation at JSC "Medicine" (Clinic of Academician Roitberg):
at the first stage, the patient is shown surgical treatment in the amount of right-sided hemicolonectomy;
continue to correct anemia;
send removed material to IHC (k-ras, n-ras);
take a blood test for NSE taking into account the assumption made by morphologists about the possibility of a neuroendocrine tumor.
04/15/16. Performed a median laparotomy, right-sided hemicolonectomy with the formation of a manual ileotransverse anastomosis of the "end-to-side" type, drainage of the abdominal cavity.
An adjuvant XELOX chemotherapy is indicated every 21 days for 6 months.
The postoperative period was uneventful, the drains were removed, the wound heals by primary intention. Anesthesia (KETOROL, tramadol), antihypertensive therapy (Prestans, Physiotens), AB-therapy (Rocefin, Metrogyl), PE prophylaxis (FRAXIPARIN, Elastic bandaging), infusion therapy (sterofundin, KMA solution), parenteral nutrition (nutotransfusion) , plasma transfusion.
The patient was discharged from the clinic at will for outpatient observation. Visiting a surgeon in 4 days.
IHC - immunophenotype and the histological structure of the tumor corresponds to colorectal carcinoma (G-2).
Dynamic surveillance
Recommended dynamic observation by an oncologist with control after 6 months:
laboratory control: hemoglobin, leukocytes, leukocyte formula, platelets;
general urine analysis;
b / x blood - glucose, total protein, urea, creatinine, ASAT, ALAT, total bilirubin, C-reactive protein, D-dimer;
tumor markers CA19-9 and CEA;
Abdominal ultrasound, colonoscopy, PET / CT.
Dynamic control one year after the end of chemotherapy (colonoscopy, PET / CT) showed no signs of residual tumor, no recurrence of the disease.