Conservative treatment of complex cardiac arrhythmias and conduction disturbances in a patient with myocardial infarction
Conservative treatment of complex heart rhythm and conduction disturbances in a patient with myocardial infarction
Sokolov Denis Vladimirovich, PhD, doctor-cardiologist.
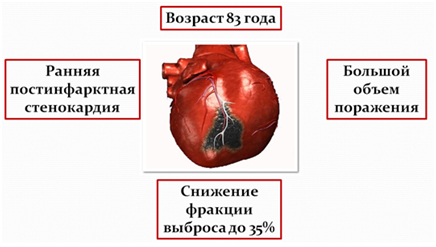
Patient I., 83 years old.
Patient complaints upon admission on 02.01.2018
· An attack of palpitations, accompanied by a feeling of shortness of breath.
Compressing pains behind the sternum, in the left and right half of the chest, of a permanent nature, radiating to the neck.
Medical history.
For more than 30 years he has noted an increase in blood pressure with a maximum increase of up to 200/100 mm Hg. Art. Adapted to 130-120 / 80 mm Hg. Art. Taking combined antihypertensive therapy.
In 2010, during examination in Munich (Germany), an aneurysm of the abdominal aorta was diagnosed, stenting was performed (two stents). During the preoperative examination, coronary angiography was performed - no hemodynamically significant lesions of the coronary arteries were revealed.
On 03.12.2017, he had an acute Q-forming myocardial infarction of the anterior wall of the left ventricle. He was treated at the place of residence in the Chechen Republic.
According to survey data from 12.2017:
EchoCG - hypokinesis of the anterior septal region of the left ventricle;
FV 36-37%;
ECG - sinus, cicatricial changes in the anterior wall of the left ventricle.
The course of myocardial infarction was complicated by early postinfarction angina from 08.12.2017.
Selective coronary angiography was not performed.
Complicated course of myocardial infarction.
Comorbidities.
Hypertension stage III. Arterial hypertension of 1 degree. Left ventricular hypertrophy (left ventricular myocardial mass index 143 g / m 2 ). Risk 4.
Aneurysm of the abdominal aorta (2 stents were installed in 2010).
Selective coronary angiography since 2010 - no significant pathology.
Gout.
Diabetes mellitus type 2.
Diabetic nephropathy with the development of renal failure ( creatinine clearance 42 ml / min / 1.73 m 2 ).
Spondylosis of the spine, lumbosacral spine. Posterior discoosteophytic complexes in the L1-S1 segment. Stenosis of the spinal canal at the L1-S1 level.
Data from previous instrumental examinations.
Echocardiography dated December 27, 2017 - areas of hypokinesis with elements of dyskinesis of the anterior, middle, apical segments, hyperkinesis of the lower parts of the left ventricle, a decrease in the ejection fraction to 35-37%.
CT scan of the chest from 27.12.2017 - effusion in the right pleural cavity (about 160 ml), hypoventilation changes in the right lung. Pneumofibrous changes in the lungs on both sides. Lymphadenopathy of the intrathoracic lymph nodes. Pulmonary hypertension. Aortocoronarosclerosis.
MSCT of the coronary arteries from 28.12.2017 - CT-picture of pronounced lesions of the coronary arteries (IV group according to Agatston).
CT signs of stenosis of the main trunk of the LCA by 38% in area, 10% in diameter, in the proximal segment of the LAD by 54% in area (27% in diameter), occlusion of the LAD in the distal segment.
Extended DV stenosis up to 72% in area (47% in diameter); the mouth section of the OA by 55% in area and 43% in diameter, the middle segment of the OA by 50% in area (40% in diameter); the proximal RCA segment by 68% in area (45% in diameter), the middle segment by 30% in area (21% in diameter), the distal segment by 25% in area (11% in diameter).
CT signs of impaired left ventricular contractile function. CT signs of left ventricular hypertrophy. Calcification of the aortic valve cusps.
Outpatient drug treatment.
Concor 2.5 mg ½ tablet in the morning.
Aspirin Cardio 100 mg 1 tablet in the evening.
Plavix 75 mg after lunch.
Crestor 20 mg at bedtime.
Valsartan (diovan) 80 mg ½ tablet in the morning.
Verospiron 50 mg before lunch.
Diuver 5 mg 1 tablet in the morning.
Allopurinol 300 mg in the morning.
Deterioration from 01/02/2018, when at about 5 a.m. he noted an attack of heartbeats, accompanied by a feeling of shortness of breath, constricting pains behind the sternum, in the left and right half of the chest, of a constant nature, radiating to the neck.
Hospitalized in the intensive care unit of the clinic of JSC "Medicine".
Status Praesens on admission.
General condition: severe. The severity of the condition is due to a violation of the heart rhythm and pain syndrome. Body temperature 36.2 ° C. Height 168 cm, weight 102 kg. BMI 37.4.
Skin: moderately pale, warm, dry. Visible mucous membranes: pink, clean, moist, shiny. Musculoskeletal system without visible pathology. Swelling of the feet.
Respiratory organs: breathing is free through the nose. Respiration rate 20 per minute. The rib cage is cylindrical in shape, evenly participates in the act of breathing. Painless on palpation. On auscultation: vesicular breathing, somewhat weakened in the lower parts of the lungs on both sides. No wheezing. SpO2 94% when breathing air.
Circulatory organs: there is no pathological pulsation in the region of the heart, vessels of the neck and epigastrium. On auscultation, heart sounds are muffled, rhythmic. Heart rate 138 per minute. According to the cardiac monitor, supraventricular tachycardia. The pulse is rhythmic, satisfying filling and tension. BP 110/70 mm RT. Art.
Digestive organs: tongue moist, clean.
The abdomen is increased in volume due to the subcutaneous fatty tissue, is not swollen, and participates in the act of breathing evenly. On palpation, it is soft, painless. Auscultatory peristalsis is heard, weakened. There was no chair today.
Urinary organs: urinates independently. The kidney area is not visually changed.
Results of examinations at admission - ECG.
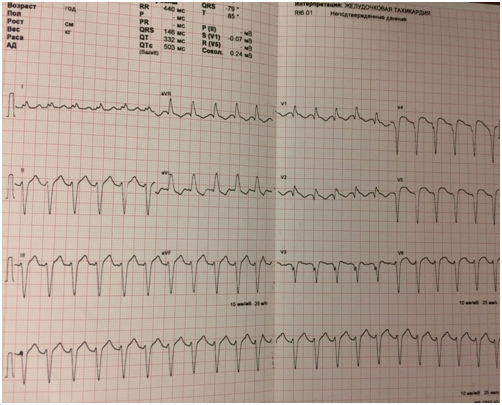
Examination results upon admission.
Clinical and biochemical blood tests without significant pathology, the level of cardiospecific enzymes is normal, the level of blood electrolytes is normal.
Echocardiography - hypokinesis with elements of dyskinesis of the anterior, middle, apical segments, hyperkinesis of the lower, ejection fraction at the level of 37-39%.
Dilation of the left heart chambers: EDC 5.8 cm, EDC 4.9 cm, EDV 167 ml, CSR 114 ml. Grade 1-2 aortic regurgitation, grade 2 mitral regurgitation, grade 2 tricuspid regurgitation.
Chest X-ray - signs of right-sided hydrothorax up to 8 ribs.
Computed tomography of the chest organs - in comparison with CT from December 27, 2017 - positive dynamics of effusion in the right pleural cavity, hypoventilation changes in the right lung. There are now traces of effusion in the left pleural cavity. Without significant dynamics: pneumofibrotic changes in the lungs on both sides. Lymphadenopathy of the intrathoracic lymph nodes. Pulmonary hypertension. Aortocoronarosclerosis.
Treatment of rhythm disturbances.


Choosing an antiarrhythmic drug?

Medication.
IV heparin 1 thousand units per hour under the control of APTT, followed by replacement with subcutaneous administration of clexane 0.4 ml per day.
IV Cordaron 300 mg bolus, then 50 mg per hour, followed by cancellation.
Use of cardiac glycosides.
The planned therapy was continued:
Aspirin Cardio 100 mg per day.
Plavix 75 mg per day.
Crestor 20 mg per day.
Valsartan (diovan) 80 mg ½ tablet per day.
Veroshpiron 50 mg per day.
Diuver 5 mg per day.
Allopurinol 300 mg per day.
Sugar-lowering therapy - IV insulin according to the level of glycemia.
On January 4, 2018, against the background of the infusion of cordarone and cardiac glycosides, a stable restoration of sinus rhythm was registered.
Conclusion of the consultation from 04.01.2018
On January 4, 2018, the patient's sinus rhythm was restored against the background of complex therapy. The course of myocardial infarction was complicated by the formation of a two-bundle blockade (in dynamics, a pre-existing blockade of the anterior-superior branch of the left bundle branch and the first blockade of the right bundle branch were noted). When the sinus rhythm is restored, the PQ interval is at the upper limit of the norm, which suggests the presence of AV block of the 1st degree, probably against the background of the involvement of the upper parts of the conducting system in the zone of myocardial infarction.
Temporary electrocardiostimulation is absolutely shown to the patient (due to the risk of aggravation of conduction disturbances along the conductive system up to complete AV blockade). The issue of resynchronization therapy will be considered in 10 days, given the positive dynamics against the background of drug treatment.
Joint discussion of 09.01.2018
The patient's condition is relatively satisfactory. No complaints. There is a stable restoration of the heart rhythm. No AV block, PQ 0.19. There are no signs of circulatory failure. In the lungs, wheezing is not heard. No cyanosis of the lips. Ejection fraction 38%. The ECG shows the dynamics characteristic of the underlying disease.
The question of the further management of the patient was raised for discussion of the council :
1. Continue outpatient therapy with follow-up.
2. Conducting coronary angiography (including at the request of relatives).
3. Installation of a resynchronizing device, incl. with further selective coronary angiography.
Recommended :
1. Further digitalization.
2. Transfer to outpatient treatment.
3. Solving the issue of resynchronization therapy.
Points of control :
1. Deterioration of A-V conductivity (currently PQ interval 0.19 with a maximum allowable value of 0.21).
2. Nausea or lack of appetite and, on the other hand, worsening circulatory failure.
3. Echocardiography is advisable to do in 2-3 weeks to determine the ejection fraction in the first place and the formation of an aneurysm.
Given the good effect on the background of the therapy, the effectiveness of cardiac glycosides, the absence of an increase in AV blockade (PQ 0.20) and the rather high operational risks in the coming months, it is recommended to continue therapy, including cardiac glycosides, and add diuretics if necessary.
Taking into account the age, severity of the patient's condition and concomitant pathology, it was decided to postpone the installation of the resynchronization device until the effectiveness of the therapy is evaluated.
This tactic of patient management does not include extreme situations, including the appearance of syncope, AV block, and complex rhythm disturbances.
With the development of life-threatening situations, an emergency selective coronary angiography will be performed to resolve the issue of the type of revascularization of the coronary arteries, followed by the choice of surgical methods for treating cardiac arrhythmias (implantation of a resynchronizing device or performing radiofrequency ablation).
The dynamics of the condition during treatment.
· Stable restoration of sinus rhythm.
· Regression of manifestations of circulatory failure.
· The patient became more active and was transferred to the department.
ECG at discharge - sinus rhythm, no rhythm disturbances were registered, ST elevation up to 1-1.5 mm V2, V3, V4, V5, V6 is preserved.
Echocardiography at discharge - the zones of left ventricular akinesis are preserved, there is an increase in ejection fraction up to 46-47%.
· Holter ECG monitoring - ventricular monomorphic ectopic activity, consisting of 565 (0.6%) contractions, of which 4 were in couplets, 539 were in single beats, 22 were trigeminic.
Supraventricular ectopic activity consisted of 2032 (2.3%) contractions, of which 14 belonged to 4 groups.
· During the study, episodes of deceleration of A-V conduction were recorded. Ischemic ST changes were not found.
Clinical diagnosis.
Multifocal atherosclerosis.
Coronary heart disease. Acute Q-forming myocardial infarction of the anterior wall of the left ventricle dated 03.12.2017.
Violation of the rhythm and conduction of the heart: for the first time revealed paroxysm of supraventricular tachycardia from 01/02/2018, arrested on 01/04/2018; supraventricular extrasystole; ventricular premature beats.
Blockade of the anterior branch of the left bundle branch. Right bundle branch block.
Hypertension stage III. Arterial hypertension of 1 degree. Left ventricular hypertrophy. Risk 4.
Aneurysm of the abdominal aorta, condition after stenting from December 2010.
Insufficiency of blood circulation II B stage. NYHA Functional Class III.
Diabetes mellitus type 2 (target level of HBA1c up to 7.0%).
Nodular non-toxic goiter. Euthyroidism.
Exogenous constitutional obesity of the 2nd degree.
Topic gout, chronic course.
Recommendations for discharge on 17.01.2018
Aspirin Cardio 100 mg 1 tablet in the evening.
Plavix 75 mg after lunch.
Digoxin 0.25 mg ½ tablet before lunch.
Crestor 10 mg at bedtime.
Valsartan (diovan) 80 mg ½ tablet in the morning according to the level of blood pressure.
Veroshpiron 50 mg before lunch under the control of the level of potassium in the blood plasma.
Diuver 5 mg 1 tablet in the morning.
Allopurinol 300 mg in the morning (in terms of a possible replacement for adenuric 80 mg in the morning).
Diabeton MB 60 mg 1 tablet before breakfast.
The future fate of the patient.
03/06/2018, a patient in a stable state underwent selective coronary angiography followed by coronary artery bypass grafting; simultaneous radiofrequency ablation for paroxysmal supraventricular tachycardia.