Education of the right lung
Analysis of the clinical case presented
doctor-therapist of JSC "Medicine" (clinic of academician Roytberg), member of the European Respiratory Society
Patient A. 49 years old.
First meeting with a patient
The patient complained about:
-
dry cough;
-
periodic bouts of difficulty breathing and a feeling of "swelling" in the neck;
-
periodic occurrence of a feeling of "difficult" inhalation;
-
when positioned on the right side, there is a feeling of wheezing in the chest on the right.
The patient does not associate the onset of seizures with provoking factors.
Some data from the anamnesis
Smoked for 15 years: from several cigarettes to 1 pack per day; does not smoke since 2012
In the summer of 2017, he began to notice the onset of shortness of breath in the form of "compression" of the chest.
Since the summer of 2017, attacks of unproductive coughing began to occur, which passed within a minute.
Follow-up by a pulmonologist at the place of residence
-
Radiography of the lungs - no pathology.
-
Foradil Combi 12/200 appointed.
-
On the background of the prescribed therapy, an improvement in well-being was noted.
Further course of the disease
In connection with the resumption of attacks of unproductive cough and the appearance of attacks of difficulty breathing at night, he again turned to the pulmonologist at the place of residence.
Spiriva was added to the therapy (1 capsule per day). No improvement in well-being was noted.
The patient was admitted to the City Clinical Hospital.
Hospitalization, February 2018 (data presented from an extract)
Survey carried out:
-
in the general analysis of blood, an increase in the number of eosinophils is noted; for other indicators - a variant of the norm;
-
the function of external respiration was studied: FVC, FEV1 - more than 80%, FEV1 / FVC - more than 70%. Salbutamol test + 8%;
-
with bronchoscopy - diffuse bilateral atrophic bronchitis;
-
the hospital underwent a comprehensive examination and bronchodilator therapy;
-
discharge diagnosis - chronic bronchitis.
Change in condition and clinical picture
After discharge from the hospital, when coughing in sputum, he began to notice dark red streaks.
He began to notice periodic rises in body temperature up to 37.2 ° C.
CT scan of the chest organs was prescribed.
CT scan from 02/26/2018
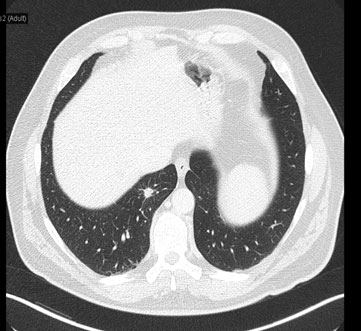
Further actions
CT scan of the chest organs shows a 19 × 15 × 27 mm mass in the S7 of the right lung, several strands directed towards the costal pleura are determined.
Consulted by a phthisiatrician - no data were obtained for the tuberculous process, a Mantoux test was carried out (reaction - 10 mm).
PET / CT
In S7 of the right lung in the basal regions, a formation with uneven tympanic contours (size 12 × 8 mm), with a low accumulation of RFP SUVmax 1.9 is determined. PET / CT image of formation in the lower lobe of the right lung with low FDG metabolism, biopsy is recommended. No other formations and foci of pathological FDG metabolism were identified.
Thus, CT scan revealed a mass in the medial basal segment of the right lung in a 49-year-old patient.
Taking into account the clinical picture, it was suggested that there was an inflammatory destructive process in the lung (abscess).
A decision was made to conduct a trial 3-week course of anti-inflammatory therapy with broad-spectrum antibiotics, followed by CT control.
Treatment
Prescribed a course of antibiotic therapy - Levofloxacin (Tavanik) 1,000 mg / day.
Against the background of therapy, the condition returned to normal, there were no changes in laboratory parameters.
A month later, a control CT scan of the chest organs was performed.
CT of the chest organs in dynamics
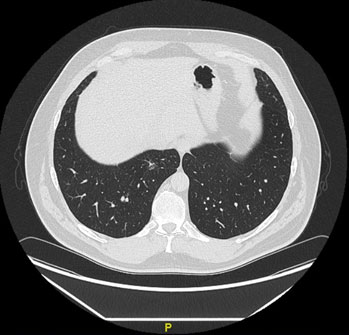
CT conclusion
The detected formation in the S7 of the right lung is not currently visualized, there is a stellate area of fibrosis with a local compaction of 3 mm with a thickening of the interlobular and intralobular interstitium.
Outcome of the disease
After the treatment:
-
the clinical picture has regressed;
-
drug therapy is not performed.