The Role of Re-Biopsy of Colonic Masses
Patient N. 54 years old
• Past diseases - measles in childhood.
• Surgical interventions: 1995 - fibroma of the left breast.
• Gynecological history - menopause 2 years, 1 pregnancy, 1 childbirth.
• History - varicose veins n / a, osteochondrosis of the cervical spine.
• Allergic history is not burdened.
• Heredity: mother - stomach cancer, father - stroke.
Went to the gynecologist with complaints of discomfort in the lower abdomen, pain. Also went to the urologist with complaints of frequent urination with a cut.
During examination:
• Ultrasound of the pelvic organs:
echographic picture of the volumetric formation of the right ovary, uterine fibroids, signs of polyps of the cervical canal.
• Complete blood count: hemoglobin 129.10 g / l;
erythrocytes 4.30 × 10 12 / l;
hematocrit 36.41.
• General analysis of urine: echrythrocytes unchanged 1.2.
• ECG, chest x-ray without pathology.
Esophagogastroduodenoscopy
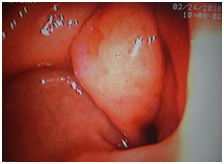 The outlet section of the stomach is clearly deformed due to tumor-like formation up to 4 cm, examination is somewhat difficult due to localization and deformation of the lumen, an ulcerative defect in the center up to 10 mm with a fibrin-covered bottom is determined.
The outlet section of the stomach is clearly deformed due to tumor-like formation up to 4 cm, examination is somewhat difficult due to localization and deformation of the lumen, an ulcerative defect in the center up to 10 mm with a fibrin-covered bottom is determined.
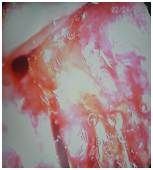
A biopsy was performed for histological examination; the mucous membrane during biopsy is rigid, cartilaginous, fragmented, bleeding markedly.
Conclusion. Tumor-like formation of the antrum of the stomach with the transition to the pylorus with deformation and slight narrowing of the lumen, biopsy.
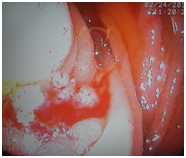
Colonoscopy
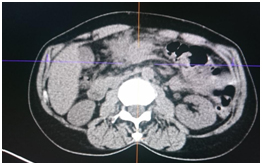
In the area of the transverse colon, a large stenosing circular formation of up to 5 cm is determined, narrowing the intestinal lumen to 1 cm, it bleeds with contact, it is difficult to pass the apparatus. A biopsy was performed for histological examination (using a guidewire for better positioning of the apparatus).
• On histological examination of the stomach formation.
Chronic superficial moderately expressed inactive gastritis with foveolar periulcerous hyperplasia, adenoma with ulceration. There are no convincing signs of malignant growth in the volume of the studied material.
• On histological examination of the formation of the colon.
Fragments of tubulo-villous adenoma with foci of severe dysplasia.
• Tumor markers:
CEA - 160.6
CA 19.9 - 884.7
CA-125 - 156.0
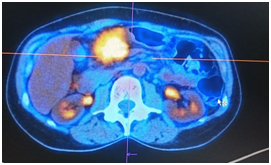
PET / CT
The hypermetabolic process in the thickened walls of the colon and the surrounding tissue may correspond to the tumor process.
In connection with the results of histological examination,
it was decided to re-examine
with a biopsy. Completed in 3 days.
Histological examination of the stomach formation.
Within the material delivered for the study, the morphological picture of moderate chronic gastritis with hyperplasia of the integumentary fossa epithelium, areas of significant edema, foci of fibrosis of the stroma of the lamina propria. No tumor growth was found within this material.
This result of histological examination was expected due to the fact that this tumor is an invasion of a tumor of the transverse colon, as can be seen on the images, and, most likely, at the time of examination there is no invasion of the gastric mucosa.
Histological examination of the formation of the colon.
In one of the presented fragments - fibrous tissue with complexes of infiltrative mucinous adenocarcinoma (G1).
Conclusion
This clinical case is interesting in that, despite the number of biopsy fragments (in total, more than 14 fragments were taken in two studies), targeted biopsy from foci of the most altered unstructured mucosa with areas of depression and impaired vascular pattern, as well as the use of biopsy forceps with volumetric branches for multiple biopsy with a storage device, there are difficulties in diagnosing lesions due to mosaic histological structure of the tumor, even of large lesions of the gastrointestinal tract, sometimes requiring repeated endoscopic studies.
Colon cancer (CT) is one of the most common malignant neoplasms.
According to the statistics of the last decade, the morbidity and mortality rates of patients with RTK are steadily growing in Russia and economically developed countries.
So, from 2003 to 2018. the growth of malignant neoplasms of the colon was 25.41%.
The frequency of metastatic ovarian tumors (Krukenberg metastasis), according to various authors, ranges from 4.18 to 63% of all malignant tumors of this organ. Most often, tumors of the female reproductive system, breast and tumors of the gastrointestinal tract metastasize to the ovaries.
Metastases in the ovaries with colon tumors are, according to various authors, from 1.7 to 12% of cases. The incidence of multiple primary malignant neoplasms (PMN) of the ovaries and colon ranges from 0.8 to 12.6%.
The clinical picture of RTK with metastases to the ovaries is not very pronounced.
With a common process, there is a violation of the function of the ovaries, pain in the lower abdomen and an increase in its volume, disorders of the function of adjacent organs (violation of urination), general disorders.
For early diagnosis of ovarian damage, the diagnostic algorithm should include the determination of the level of tumor markers CEA, CA 19-9, CA 125, ultrasound of the pelvic organs and the abdominal cavity.
Literature.
1. Emelyanov S.I., Uryadov S.E. Colonoscopy for polyps and colon cancer (literature review). Endoscopic Surgery 2010; 4: 18-23.
2. Казакевич В.И., Митина Л.А., Востров А.Н., Гуц О.В. Ультразвуковая диагностика метастатического поражения яичников при раке желудочно-кишечного тракта. Ультразвуковая и функциональная диагностика 2009;5:14. [Kazakevitch V.I., Mitina L.A., Vostrov A.N. Guts O.V. Ultrasound diagnosis of metastatic disorder of ovarian in cancer of the gastrointestinal tract. Ultrazvukovaya i funktsionalnaya diagnostika = Ultrasound and functional diagnostics 2009;5:14 (In Russ.)].
3. Meyerhardt J., Sanders M. Colon cancer. -M: LLC "Reed Elsiver"; 2009.
4. Казаков М.П., Поддубная И.В., Любченко Л.Н., Харитонова Т.В. Наследственный рак яичника (литературный обзор). Современная онкология 2012;1(14):47–54. [Kazakov M.P., Poddubnaya I.V., Lubchenco L.N., Kharitonova T.V. Hereditary ovarian cancer (literature review). Sovremennaya onkologiya Modern oncology 2012;1(14):47–54 (In Russ.)].
5. Prorokov V.V., Malikhov A.G., Knysh V.I. Modern principles of diagnostics and screening of rectal cancer. Practical Oncology: Selected Lectures. – St. Petersburg; 2004; 162-167.
6. Попова Т.Н. Диагностика и лечебная тактика у больных с первично-множественными синхронными злокачественными опухолями. Дис. д-ра мед. наук. М., 2002. [Popova T.N. Diagnosis and treatment strategy in patients with multiple primary synchronous malignant tumors. Thesis ... Dr. sci. med. M., 2002 (In Russ.)].
7. Uryadov S.E. Diagnostic and therapeutic colonoscopy. - M: Panfilov Publishing House; 2010.
8. Kim D.D., Park I.J., Kim H.C. et al. Ovarian metastases from colorectal cancer: a clinicopathological analysis of 103 patients. Colorectal Dis 2009 Jan;11(1):32–8.
9. Omranipour R., Abasahl A. Ovarian metastases in colorectal cancer. Int J Gynecol Cancer 2009 Dec;19(9):1524–8.
10. Simon M.S., Petrucelli N. Hereditary breast and ovarian cancer syndrome: the impact of race on uptake of genetic counseling and testing. Methods Mol Biol 2009;471:487–500.
11. La Vecchia C. Epidemiology of ovarian cancer: a summary review. Eur J Cancer Prev 2001;10:125–9.
12. Regula J., Rupinski M., Kraszewska E., Polkowski M., Pachlewski J., Orlowska J. Colonoscopy in colorectalcancer screening for detection of advanced neoplasia. N. Engl. J. Med. 2006; 355:1863–1872.