Absence

Physician-therapist, somnologist
Novikov Maxim
Experience 13 year
Doctor of the highest category. Member of the European Respiratory Society and the Russian Respiratory Society
Absences are a group of epileptic pathologies characterised by brief loss of consciousness without a seizure attack. Patients experience muscle tone disorders and this syndrome may be combined with other forms of organic lesions of the human brain. The degree of tissue damage is determined after the patient undergoes a cerebral MRI scan. Treatment is supervised by epileptologists and neurologists.
Disease pathogenesis
The mechanics of the formation of absences have not been established. Clinical studies have identified that the cerebral cortex and thalamus play a significant role in the development of this pathology. A common assumption among neurologists is that the disease is formed under the influence of genetic factors that create conditions for the development of atypical characteristics of neurons.
Typical absence occurs against a background of inhibitory activity, which is the patient's response to hyper-excitement. Atypical cortical activity becomes a compensatory mechanism that aims to suppress pathological excitation. Childhood absences disappear by the age of 18-20, due to the completion of brain development.
Developmental causes
Pathological seizures are based on an imbalance between inhibition and excitation processes in the cerebral cortex. Epileptic absences are divided into two groups: secondary and idiopathic.
Secondary (typical) absences are caused by encephalitis, cerebral abscess, brain tumour. The pathology becomes a consequence of the underlying disease - its manifestations cease after successful treatment.
Idiopathic (atypical) absences are formed for unexplained reasons. Assumptions about their genetic nature are supported by family histories with numerous cases of epilepsy. The risk group includes children aged 4-10 who suffer from febrile seizures.
Among the reasons provoking the development of absences are:
- sleep deprivation;
- mental and physical overload;
- excessive visual stimulation;
- hyperventilation of the lungs.
Deep forced breathing is seen in 90% of patients suffering from this pathology.
Disease classification
Types of absences are distinguished on the basis of the clinical picture (presence or absence of muscle and motor disorders in the patient). The type of pathology can be diagnosed after visual observation of the seizure. Complex absences are accompanied by changes in a person's muscle tone for 10-20 seconds. Muscle-motor episodes form several subtypes of the pathology: atonic, myoclonic, tonic and automatic.
A simple absence develops as a one-time blackout of the mind of a person suffering from this pathology for 25-30 seconds. There are no other symptoms or signs of the disease. A flash of light or a loud sound helps to bring the patient out of an absent minded state. Mild forms of the illness allow the person to continue the dialogue or actions interrupted by the seizure.
Symptoms

The main symptom is a paroxysmal seizure lasting about 30 seconds. Patients lose conscious awareness of their surroundings. Eyewitnesses to such episodes may observe an absent look and a look of bewilderment on the face of the person carrying this pathology. Brief freezing in one posture is possible. Mild absences allow the person to continue the interrupted activity at a slower pace, severe absences cause the activity to be stopped.
People with organic brain damage describe seizures as a lapse, a falling out of reality, a trance-like state. The end of the attack is not accompanied by a deterioration in their well-being. Brief episodes of typical absences may remain unnoticed.
Complex absences are easier to detect because of the motor and tonic manifestations. Often there is a decrease in a patient's muscle tone, which leads to dropping the arms, tilting the head and sliding down from the chair. Complete atony provokes a fall with the risk of injuries.
Complications
Epileptic status occurs in one-third of patients suffering from absences. The period of a complicated seizure may last from two to eight hours. The person is in a state of confusion, thought processes are extremely slowed down and behavioural disorders are noted. Speech becomes incoherent and phrases are short and simple.
Atonic absences often lead to injuries due to patients' fallings. Characteristic injuries are contusions, dislocations, fractures and craniocerebral injuries. The most serious complications are mental retardation, manifesting as oligophrenia or dementia. Their development is not due to absences, but to systemic lesions in the human body.
Appointment
Detection of the first symptoms of epileptic absences by relatives and friends is a good reason for a visit to the clinic. Any stages of the disease require consultation with a neurologist or an epileptologist. During the diagnosis and treatment of the disease, patients may need opinions from other specialists: a general practitioner, a cardiologist, a surgeon.
Diagnostics
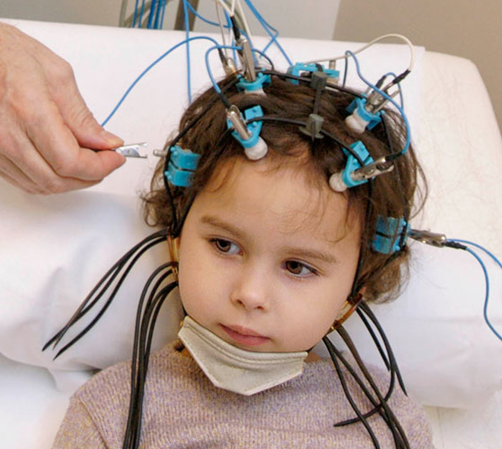
The aim of the diagnostic procedures is to find out whether the patient has absences and to identify the illness that causes them. The person with the disorder will have to:
- be seen by a neurologist. – in rare cases, mental retardation and cognitive impairment are diagnosed;
- carry out an electroencephalography – this procedure provides a record of the brain's bioelectrical activity at the time of an artificially induced paroxysmal seizure;
- have a brain MRI – scans confirm or refute the presence of organic pathology that causes epileptic activity.
A set of diagnostic measures provides detection of cerebral tuberculosis, encephalitis, tumours, or brain abnormalities. The treatment strategy is formed taking into account the initial cause of the absences.
Treatment
Treatment for a combination of absences and other seizures involves the prescription of anticonvulsants. These medicines are effective in preventing the development of paroxysms. Normal absences are treated with ethosuximide, a low-toxicity anti-epileptic spectrum medicine. The daily dose is determined on the basis of the patient's age, weight and clinical picture of the pathology.
Side effects of anti-epileptic medicines include gastrointestinal disorders, headaches, dizziness and skin damage caused by dermatitis. For this reason, medicines should only be prescribed after a full cycle of diagnostic tests. Patients’ self-administration of pharmacological preparations can provoke depression of central nervous system functions and respiratory organs.
Treatment of collateral injuries that occurred when the patient fell during a seizure is performed by a general practitioner, trauma surgeon, or surgeon. Painkillers are prescribed according to the pharmacotherapy of the underlying disease to rule out incompatibility of the active ingredients.
How to make an appointment?
You can make an appointment with all specialists at JSC "Medicina" (Academician Roytberg Clinic) on the website - an interactive form allows you to select any doctor by specialty or search for any employee of any department by name and surname. Each doctor's schedule contains information about the opening days and hours available for appointments.
Our clinic's administrators can make an appointment or make a house call by calling +7 (495) 266-95-40.
Our convenient location in the Central Administrative District of Moscow (CAD) - 2nd Tverskoy-Yamskoy Lane, 10 - allows you to quickly get to the clinic from several metro stations: "Mayakovskaya", "Novoslobodskaya", "Tverskaya", "Chekhovskaya" and "Belorusskaya".