Myocardial perfusion scintigraphy
Patient Ch. 57 years old.
Went to a cardiologist with complaints of instability of blood pressure and a feeling of interruptions in the work of the heart.
Medical history.
In childhood - tonsillitis (with frequent relapses). He has noted increases in blood pressure over the past 10 years, constantly takes Betalok Zok (daily dose of 5 mg) and Gizaar (daily dose - 50 / 12.2 mg); interruptions in the work of the heart for five years, takes Etatsizin (daily dose 100 mg); since 2004 suffers from type 2 diabetes mellitus, was on insulin therapy, after weight loss, therapy was revised and Amaryl 4 + 2 mg was prescribed in the morning before meals, Glucophage 1000 1 tablet in the morning and evening, Byetta 10 mg 2 times a day p / to.
During the survey:
Laboratory examination: complete blood count - no changes, lipid spectrum - within the norm. Glycosylated hemoglobin - 6.2%, glucose - 7.9 mmol / l.
ECG. Sinus rhythm, normosystole. The electrical axis of the heart is deflected to the left. Features of intraventricular conduction.
ECHO-KG. Compaction of the walls of the aorta, aortic valve leaflets, mitral valve leaflets without hemodynamically significant dysfunction. Slight dilatation of the ascending aorta. Slight dilatation of the left atrium. Concentric hypertrophy of the left ventricular myocardium to a significant degree without signs of obstruction of the left ventricular outflow tract at rest. Global myocardial contractility is normal. Local myocardial contractility is not impaired. Violation of left ventricular diastolic function without an increase in end-diastolic pressure. Small hydropericardium.
Treadmill test.
Test: negative. Load Tolerance: Medium.
Type of hemodynamic response to exercise: hypertensive.
MSCT. MSCT picture of a balanced type of coronary blood supply. Severe coronary sclerosis. Indirect signs of arterial hypertension. Stenoses: RCA 30-40%; PNA up to 40%; mouth of DA up to 50%. S-shaped deformation of the PCA in the middle segment. Left ventricular myocardial hypertrophy.
Comments: at the height of the load and in the recovery period, no changes in the ST segment of the "ischemic type" of anginal pain were registered. In the recovery period, polymorphic ventricular premature beats were registered.
Physical examination data. The condition is satisfactory. No edema. With auscultation of the lungs, breathing is carried out through all departments, vesicular, no wheezing. On auscultation, the heart sounds are muffled, rhythmic, no noise. Pulse 80 beats / min., Rhythmic, satisfactory filling and tension. BP 140/90 mm Hg. Art.
Consciousness is clear, oriented in time, personality and space. There are no meningeal signs. There are no focal symptoms.
Preliminary diagnosis: ischemic heart disease. Hypertension 3 tbsp., Risk 4. Hypercholesterolemia 2 B type.
Survey plan. Taking into account the data of MSCT of the coronary arteries (pronounced coronary sclerosis), a high risk of developing atherosclerosis in the absence of signs of myocardial ischemia according to the ECG, echocardiography, treadmill test, additional examination is indicated: perfusion myocardial scintigraphy with stress.
Myocardial perfusion scintigraphy .
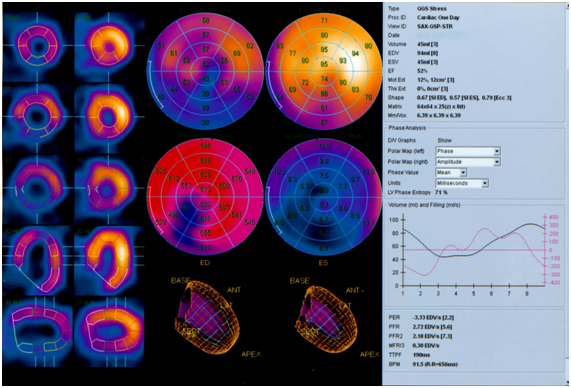
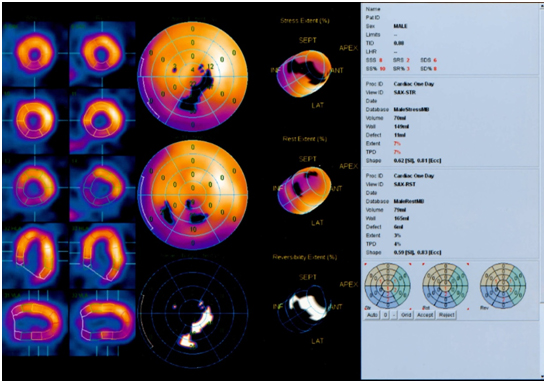
On scintigrams at rest, the site of RP hypofixation in the myocardium of the left ventricle in the region of the lower apical segment and the apex segment of the lower wall is determined (2 segments, 3% of the myocardium, 1-2 degrees).
After the stress test (veloergometry), the RFP hypofixation area extends additionally to the middle segment of the lower wall, the anterior and lower apical segments of the lateral wall, the anterior apical segment of the septum (6 segments in total, 7% of the myocardium, grade 1-2).
Indicators of global systolic function of the left ventricle are within normal limits: EDV - 94 ml, CSR - 45 ml, ejection fraction 52%, peak ejection rate 3.33 EDV / s.
The amplitude of contractions and the degree of systolic thickening of the myocardium in the region of the lower wall of the left ventricle are moderately reduced.
Reduced filling rate of the left ventricle in the first third of diastole.
Conclusion.
Scintigraphic signs of a mixed perfusion defect of the left ventricular myocardium (permanent perfusion defect in the lower apical segment and the apex segment of the lower wall, transient perfusion defect in the middle segment of the lower wall, anterior and lower apical segments of the lateral wall, anterior apical segment of the septum). There were no violations of the global systolic function of the left ventricle, signs of local hypokinesia in the region of the lower wall. Signs of diastolic dysfunction.
A permanent perfusion defect is regarded as an area of cardiosclerosis, a transient perfusion defect as an area of stress-induced myocardial ischemia.
Based on the data of myocardial perfusion scintigraphy, the patient was diagnosed with a final diagnosis.
Final diagnosis.
Coronary heart disease. Atherosclerosis of the aorta, heart vessels. Hypertension 3 tbsp., Risk 4. NK 0 tbsp. Postmyocarditis cardiosclerosis. Type 2 B hypercholesterolemia.
Appropriate treatment was prescribed.
For reference.
Myocardial perfusion scintigraphy currently occupies a priority position in the diagnosis of coronary ischemia in comparison with other methods of heart examination, which is primarily due to the high rates of its sensitivity, specificity and information content. The non-invasive route of administration of the labeled compounds is of great importance. Diagnostic myocardial perfusion scintigraphy should be performed in patients with implicit coronary symptoms or in those with risk factors but negative tests for latent coronary insufficiency.
Clinical indications for myocardial perfusion scintigraphy:
1. Diagnosis of ischemic heart disease:
· differential diagnosis of chest pain;
· questionable ECG stress test;
· resting ECG disturbances;
· high risk of coronary artery disease without severe clinical symptoms.
2. Assessment of the severity of coronary artery disease:
· identification of multivessel coronary lesions;
· determination of the volume and localization of coronary microcirculation disorders;
· assessment of the functional state of collaterals;
· assessment of the inclusion of the indicator in the lungs.
3. Defining a treatment strategy:
· selection of patients for coronary artery bypass surgery;
· selection of patients for scar excision after myocardial infarction.
4. Examination of patients selected for coronary artery bypass grafting:
· forecast of the results of revascularization;
· assessment of myocardial viability;
· differential diagnosis between the area of the hibernated myocardium and scar tissue.
5. Evaluation of reperfusion results:
· assessment of the patency of coronary artery bypass grafts;
· determining the effectiveness of angioplasty;
· monitoring the effect of thrombolytic therapy.
6. Resting scintigraphy for acute myocardial infarction and unstable angina pectoris:
· differential diagnosis of AMI and unstable angina pectoris;
· assessment of the prognosis of coronary pathology.
The information content of the scintigraphic diagnosis of coronary artery disease is significantly increased when using stress tests. Exercise scintigraphy is of particular value when examining patients with negative results of exercise tests (bicycle ergometry, treadmill test), as well as in cases when at rest there are changes such as left ventricular hypertrophy or bundle branch block, masking ECG signs of ischemia ...